by Randy Kidd, DVM, PhD Put simply, the function of the kidneys is to make urine, a “waste” product of body metabolism. Of course, there is much more to the kidneys. They are powerful chemical factories that: • Remove waste products, toxins, and drugs from the body • Balance the body’s fluids and help maintain a constant body pH • Release hormones that regulate blood pressure and control the production of red blood cells • Produce an activated form of vitamin D that promotes strong, healthy bones Anatomy and physiology The two kidneys lie against the back abdominal wall, lateral to the spine, in the lumbar region. They are encapsulated organs, shaped somewhat like a kidney bean, and their size varies with the size of the dog. The functional unit of the kidney is the nephron. There are perhaps a million nephrons in each kidney, each one comprised of a glomerulus and a long tubule that eventually empties into the ureter.

The glomerulus is a congregation of blood vessels contained within Bowman’s capsule, and the glomeruli are located in the outer portion of each kidney (cortex). Blood is filtered as it passes through the kidney’s collection of glomeruli. After filtration in the glomeruli, the resulting protein-free fluid is passed into a thin tubule. The proximal tubule descends into the med-ulla of the kidney and then makes a sharp U-turn (at the loop of Henle) to return into the cortex, where it empties into a collecting duct, even-tually exiting via the ureter. The tubules are responsible for secretion of some substances (such as drugs and their by-products, uric acid, fatty acids, and bile salts) and reabsorption of a variety of other permeable solutes, among them glucose, amino acids, vitamins, minerals, urea, and some salts, notably sodium, chloride, and potassium. Urine passes into the bladder where it’s stored until it’s excreted via the urethra. Blood pressure is controlled by a complex interplay of hormones. In response to decreased blood pressure (as a consequence of chronic congestive heart failure or CHF, for example) the kidneys release renin. This is a proteolytic enzyme that acts on liver-produced angiotensinogen, which is converted to angiotensin I and then to angiotensin II. Angiotensin II causes retention of sodium and water, in part through stimulation of the synthesis and release of aldosterone by the adrenal cortex. Angiotensin II also causes vasoconstriction, thus increasing vascular resistance. Vasoconstriction and water retention place further stress on the already compromised heart muscles, and ultimately these conditions may also damage the kidney’s nephrons. Thus, angiotensin-converting enzyme (ACE) inhibitors are widely used in treating CHF in dogs, and many practitioners include them for the treatment of kidney disease. The maintenance of the body’s overall acid/base balance also relies on a complex mechanism that depends on adequate respiratory and digestive function as well as kidney mechanisms. The kidney’s role in keeping the body’s pH within a healthy range is related to balancing the potassium and hydrogen ion retention and depletion and is especially important during hypoxia (when the animal is not receiving enough oxygen, either from poor respiratory function and/or a diminished supply of red blood cells). The kidney is both the sensor organ and the major site for the production of erythropoietin, the hormone that regulates production of red blood cells. Chronic renal failure is thus typically accompanied with a mild to moderate anemia. Bone health is reliant upon healthy kidneys in at least two ways. First, vitamin D is necessary for the utilization of calcium, and the activated form of vitamin D is produced in the kidney. Second, normal kidneys excrete phosphorous; chronic renal failure may lead to excessive retention of phosphorous, which in turn causes an imbalance between calcium and phosphorous. Vitamin D must be metabolically activated (via hydroxylation in the liver and kidney) before it can function physiologically; the conversion in the kidneys is the rate-limiting step in vitamin D metabolism. Occasionally the imbalance of calcium to phosphorous seen with increased retention of phosphorous may create a decreased amount of circulating calcium. Parathyroid gland hyperplasia occurs (to maintain serum calcium in normal ranges), and the resultant high parathyroid hormone (PTH) concentrations result in increased bone resorption, which ultimately creates thinning of the bone. Note here that the major contributor to the softening of the bones is an imbalance between calcium and phosphorous levels in the body. Rarely, the opposite of the above condition (hypercalcemia) occurs with renal disease, but the pathogenesis of this condition is unknown. Note also that calcium metabolism is involved with bladder and kidney stone formation, which often makes for complicated therapeutic decisions whenever we need to treat kidney disease. Notes about renal disease Renal disease refers to the presence of morphologic or functional lesions in one or both kidneys, regardless of extent. Renal failure refers to the retention of nitrogenous waste products of protein metabolism, regardless of the cause. Renal insufficiency is a term that has been used to describe a state of reduced renal function that has not yet resulted in retention of nitrogenous waste products. Azotemia (from the Greek azote, meaning “nitrogen”) is defined as an excess of urea or other nitrogenous compounds in the blood. You may also hear the term “uremia” used to replace azotemia, but uremia has now come to refer to the entire constellation of signs and symptoms of chronic renal failure: nausea, vomiting, anorexia, uremic odor of breath, pruritus (itchy skin), neuromuscular disorders, pain and twitching of muscles, hypertension, edema, mental confusion, and acid-base and electrolyte imbalances. Typical causes of azotemia are classified by their location: prerenal, from diminished blood flow into the kidneys; post-renal, usually due to a blockage of the “outflow vessels” (ureters or urethra); and renal disease that can be caused by a lack of proper function of any of the components of the nephron (the glomerulus or tubules), or it can be caused by conditions affecting the tissues between nephrons. Finally, to help determine treatment, practitioners also like to know if the disease is acute or chronic, and if it appears to be progressive or nonprogressive. Diagnosis of urinary disease Noticeable symptoms and signs of urinary system disease will, of course, vary with the disease and its severity, but the following general symptoms should make you suspicious of urinary system disease. Dysuria, that is, any abnormality of urination, including polyuria (passage of large amounts of urine in a given period), may be the animal’s attempt to compensate for diminished functional capacity of the kidneys, and it is often associated with polydipsia or chronic excessive thirst. Hematuria indicates the presence of blood in the urine and may be due to renal calculi, trauma, or destruction of the red blood cells within the body (this latter condition is more correctly referred to as hemoglobinuria). Oliguria (from the Greek oligos, meaning little or few) describes the secretion of a diminished amount of urine in relation to the fluid intake, and stranguria (from the Greek stranx, meaning “drop”) describes slow and painful discharge of urine, due to spasms of the urethra and bladder. Anuria is defined as the complete suppression of urinary secretion by the kidneys. It is an emergency condition whenever urine flow has ceased, whether due to kidney shut down (shock, for example) or blockage of the outflow vessels of the urinary tract (stones). See your veterinarian immediately. If renal disease proceeds to chronic renal failure, uremia results, and (as mentioned above) uremia produces an entire constellation of signs and symptoms. Other symptoms, seemingly unrelated to the kidneys, may occur with chronic renal failure: pulmonary edema and coughing, bone conditions related to softening of the boney mass, heart conditions related to improper control of blood pressure, and symptoms related to anemia such as difficulty breathing, exercise intolerance, restlessness, etc. Symptoms, even those that become evident when specific diagnostic aids such as urinalysis and blood chemistries are employed, may not occur until a very high percentage of the nephrons are not functioning properly. Perhaps as many as 70 percent or more may need to be dysfunctional before specific symptoms are detected. Urinalysis The primary diagnostic aid for kidney disease, a typical urinalysis includes the urine’s specific gravity, its pH, and the presence of abnormal amounts of substances such as protein, glucose, and creatinine. Important findings in the urinary sediment include red or white blood cells, crystals, bacteria, or other organisms such as yeasts. A functional kidney is able to concentrate (or dilute) urine to a specific gravity that is different from that of the blood plasma (circulating blood plasma has a specific gravity of 1.010 + 2); kidney disease is diagnosed when the urine specific gravity remains at 1.010 + 2, regardless of the dog’s state of hydration. Normal pH of the carnivorous animal’s urine is acid (below pH of 7), and it typically becomes more basic with bacterial infections. The consistent presence of glucose in the urine (glucosuria) indicates the likelihood of diabetes mellitus. The presence of cells or microorganisms in the sediment are indicators of infection or inflammation. Moderate amounts of protein in the urine signify that there is a “leak” in the glomerular filtration system, that the kidneys are unable to retain proteins in the bloodstream. See “Urine Luck” (February 2004) for more information on urinalysis. Blood tests Blood chemistry tests can also help diagnose some urine system dysfunctions. Renal excretion of urea is accomplished by glomerular filtration. Urea is also reabsorbed passively in the renal tubules, which means that its blood levels will increase whenever there are slower tubular flow rates – during dehydration or blood volume depletion, for example. So, one important result of the blood chemistry test examines the blood urea nitrogen (BUN) levels. Creatinine, a product of the normal metabolism of muscles, is excreted by the kidneys by glomerular filtration. Non-renal variables, such as excessive muscular activity, muscle necrosis, and possibly ingestion of a meal of cooked meats, may have a small and transient effect on the blood creatinine level, but it is still considered a good indicator for glomerular function. Creatinine and BUN assays offer an indirect measurement of the glomerular filtration rate (GFR), which in turn is a good assessment for the overall functional capacity of the glomeruli. Phosphorous retention results from declining function of the glomerulus, and blood phosphorous levels may be extremely high with chronic renal disease. Blood albumin levels may also be low due to inadequate retention of proteins, and the decreased levels of protein may lead to edema and/or malnourishment. A mild anemia often occurs with severe kidney disease (due to improper production of erythropoietin). Elevated white cell counts may point to infections in the urinary tract. A complete blood count (CBC) can help detect these conditions. Other diagnostic tests include abdominal X-rays, contrast studies of the urinary tract, ultrasonic exams of the kidneys and bladder, and renal biopsy. Some diseases (diabetes and CHF in particular) may predispose the dog to renal failure, so tests to rule these out may be needed. See “Passing the Blood Test” (November 2003) for more information on blood chemistry analysis. Prerenal conditions These conditions result from reduced blood flow to the kidneys due to such causes as dehydration, congestive heart failure, or shock. They usually resolve completely with appropriate treatment, but they may also progress to renal disease and renal failure. Renal conditions

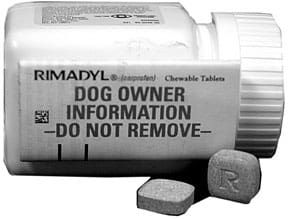
Every practitioner will tell you that kidney disease is one of the most common entities seen in vet practices daily. Acute renal failure usually occurs following a major insult to the kidneys. Potential causes include vascular conditions (such as disseminated intravascular coagulation or DIC), immune mediated conditions (such as lupus), renal infections, and ingestion of toxins (such as heavy metals, aminoglycoside antibiotics, painkillers, and ethylene glycol or antifreeze). Once the instigating factor(s) is removed with specific therapy, and supportive therapy is instituted (for example, fluids to enhance flow through the nephrons), the kidney typically returns to its normal function. If the disease process is allowed to proceed for a few days to a few weeks, chronic renal disease may ensue. Chronic renal failure (CRF) presents a far more complex and ever-evolving picture. Therapy often must be adapted to the individual case and its progress over time. Basic principles of therapy include: • Determination of the cause of the disease, if at all possible. • Removal of potential toxins – including drugs that are known to be harmful to the kidneys. • Restoration of blood flow through the glomeruli. Fluids, given sub-Q, IV, or orally if possible, can be life-saving. Some dogs with CRF can manage a fairly good quality of life so long as fluids are administered on a routine basis – daily or several times a week. • Dietary changes to help bring the body and the urinary system back into balance (see nutrition, below). • Specific treatments to help counter the cause of the disease. Infections, for example, can be treated with antibiotics, herbs, acupuncture, or immune system-enhancing methods. Primary glomerulopathies are uncommon in dogs. They are often due to an immune-mediated disease that ultimately creates the formation of immune complexes in the glomerular capillary wall. These immune complexes prevent normal glomerular functioning, and the dog is unable to retain protein. The primary symptoms are frequently due to the protein loss: weight loss, edema or ascites, dyspnea (difficulty breathing, due to pleural effusions or pulmonary edema), coagulation disorders, and proteinuria. Severe cases can result in renal failure and uremia. Drugs are a prevalent cause of renal disease, and there are many that have been implicated. Aminoglycoside antibiotics are the second most common cause of acute renal disease in dogs (behind only antifreeze toxicity), and the frequency of toxicities seems to be increasing every year. Although their spectrum of toxic severity varies, all antibiotics in the aminoglycoside classification are nephrotoxic. Aminoglycoside antibiotics include neomycin, kanamycin, gentamicin, amikacin, and streptomycin. Many painkillers (including nonsteroidal anti-inflammatory drugs or NSAIDs), chemotherapy agents, and many other drugs have been reported to be nephrotoxic. Some herbs have also been cited as potentially nephrotoxic, including wormwood (Artemisia absinthium); sassafras (Sassafras albidium); horse chestnut (Aesculus hippocastanum); chaparral (Larrea spp.); and periwinkle (Vinca minor). Bottom line: Ask about the potential renal toxicities for any drug or therapy your practitioner recommends. Postrenal conditions There are several potential causes of partial or complete obstruction of the outflow vessels of the urinary tract, including tumors, enlarged prostate in the male dog, trauma that causes blood clots or eventual scarring, and uroliths or stones. Of these, stones are the most common. Generalized symptoms of constriction of the urinary tract include nonproductive straining to urinate, increased frequency of urination (without an increased volume), and blood in the urine. Symptoms may be present for a period, followed by periods of apparently normal function. Uroliths (also known as urinary calculi or stones) are crystalline concretions, found in the urinary tract, that contain mostly inorganic crystalloids, along with a small amount of organic matrix. Almost any mineral substance that passes through the kidneys could form one of these precipitates, and under favorable conditions, a hardened concretion could develop. Stones are named according to the predominate crystal found within. The most common stones found in dogs are struvite and calcium oxalate. Typically, when a dog has uroliths, crystals are seen in urine sediment. Depending on the stone’s size and mineral composition, X-rays can be used for detection; however, some uroliths don’t show up well on X-ray films. Laboratory analysis of the stones is needed to positive identify the minerals they contain. Some breeds are predisposed to forming uroliths, and some breeds are especially prone to forming a specific type of urolith. For example, due to a genetic defect in uric acid metabolism, Dalmatians are predisposed to urate calculi formation. With each type of urolith, there are predisposing factors that tend to precipitate the problem, and each of these factors is specific for the type of urolith formed. For example, oxalate crystals form in acidic urine, struvite crystals tend to form in alkaline urine. Check with your vet for these specifics, to help formulate a plan for treatment and prevention. Symptoms vary with the location and the size of the urolith. They include frequent attempts to urinate, straining or inability to urinate, hematuria, overdistended bladder, or signs of uremia. Uroliths may also be totally or periodically asymptomatic. They often cause secondary irritation and result in infections. Struvite is composed of magnesium ammonium phosphate, in varying ratios and degrees of purity. Struvite uroliths form in alkaline, concentrated urine, and there is a genetic predisposition for their formation. Medical management may be helpful and may even dissolve the stones. A medical protocol would include enhancing urine flow (diuresis along with plenty of water intake), production of acidic urine, and dietary means to reduce magnesium and phosphorous and (perhaps) to reduce protein. (For more on protein, see nutrition section, below.) Calcium oxalate uroliths, in contrast, must be removed surgically, since attempts to dislodge them by nutritional means alone have not proven successful. An acute urinary obstruction is an emergency condition that requires immediate care. Urine backup creates a toxic level of urea in the body which may, within hours, cause neurological signs and eventually lead to death. Your veterinarian may need to use anesthesia to pass a catheter to dislodge the stone(s) for immediate relief. Other urinary tract diseases Infections of the urinary tract include cystitis (infection of the bladder), pyelonephritis (kidney infection), and urethral infections. Infections can be caused by a variety of microorganisms, and they are conventionally treated with antibiotics or alternatively with herbs or other methods. Clinical symptoms include the list of urinary dysfunctions: hematuria, difficulty and increased frequency of urination, etc. Infections are usually easily diagnosed by examining the urine sediment for the presence of bacteria and/or blood cells. Culture and sensitivity can also be performed to determine the antibiotic of choice; herbal remedies typically have a broad range of activity, although their potency may not be quite as strong. While symptoms of urinary infections or obstruction may wax and wane, depending on the degree of obstruction and/or the amount of irritation to the urinary tract, you can often predict an event by observing precursor symptoms such increased attempts to urinate (with poor results), straining to urinate, or blood-stained urine. At the onset of these symptoms, I’ve had excellent results with dandelion root (Taraxacum officinale) and Oregon grape root (Berberis aquifolium), perhaps along with echinacea (Echinacea spp.) to enhance the immune system. Of course, make sure the dog drinks plenty of water and continues to be able to urinate freely. Dandelion acts as a diuretic and Oregon grape root has antibiotic activity; the combination is often enough to ward off further development of disease while we try to correct the problem nutritionally or with other medications. There are two problems of the urinary tract – urinary incontinence and conditions of the prostate – that deserve more discussion, but since they are more related to the reproductive tract, I’ll cover them in the next installation of the Tour of the Dog. The urinary system is also affected with a long list of physical anomalies, many of which have a familial tendency. Included in this list are renal dysplasia and hypoplasia, renal agenesis, polycystic kidneys, renal cysts, and some of the glomerulopathies. Neoplastic diseases also occur along the length of the urinary tract, and their diagnosis and treatment are the same as for neoplasias affecting other sites. Western and other therapies Western medical therapies for treating urinary system diseases are aimed at the following: removing or discontinuing instigating factors (infections, for example, or nephrotoxic drugs); improving hydration so that urine flow through the tract is optimal; providing nutritional support that minimizes stress to the kidney while it helps return the body back to balance; and using specific medications that apply to the ongoing condition of the patient. Alternative medicines can be helpful for treating many of the common conditions that affect the urinary system. Alternative medicines may prove even more beneficial for maintaining a balance of the “extra” functions of the kidney – the functions that help the animal maintain homeostasis. “Alternative” or “holistic” practitioners will try to create the same benefits that their Western colleagues expect, typically by using a more natural approach – with home-prepared foods rather than commercial “prescription” diets, as one example. A holistic practitioner will also likely employ one of the alternative methods to try to re-establish homeostasis. Nutrition will likely be the mainstay for the holistic practitioner treating renal disease. Holistic treatments will vary according to individual patient needs and will likely change as the healing process progresses. Nutrition Nutritional approaches to treating urinary tract diseases are fairly common now, especially since the dog food companies have seen the potential for increased sales. It’s important to remember that each type of urinary tract disease requires an individualized nutritional approach. With this in mind, there are some basics that may help you when you devise a diet for your dog. It is important to maintain fluid flow through the kidney, so the dog’s diet should either be moist or should encourage drinking lots of water. Some diets include salt to enhance thirst, but salt encourages fluid retention, which is not good for the heart. Excess phosphorous may speed the progression of renal conditions. Low-phosphorus diets are difficult to formulate, so most commercial foods contain “phosphorous binders” – substances that contain ingredients that remove phos-phorous from the blood. Some diets or therapeutic regimes use potassium citrate, an alkalizing agent that helps maintain potassium levels in the body and helps with the management of calcium oxalate uroliths. Antioxidants (such as Omega-3 and -6 fatty acids) can speed the repair of renal damage from disease. Vitamins A, C, and E can be used for their antioxidant effects, but these vitamins can affect the pH of the dog’s urine. If your dog has a history of or predisposition to stones, work with your vet to monitor the pH of the dog’s urine when you feed these supplements. B vitamin supplements can be beneficial, especially if diuretics are used to enhance urine flow. One of the most controversial topics in canine nutrition has to do with proteins in the diet of kidney-compromised dogs. Studies have produced conflicting results. In years past, we thought that we helped compromised kidney function by providing a low-protein diet. Not all current research supports this, however. Recent studies indicate that a low-protein diet (less than about 10 percent) may actually be detrimental when treating kidney disease. What seems to be the consensus now is that a diet moderately high in protein (30 to 35 percent), provided in high quality, readily assimilated proteins, is most supportive for long-term care of the kidney-compromised dog. What none of the studies shows is what most interests a holistic practitioner: How much “vitality” is contained in the food. Processed foods have almost no healthy “energy.” Raw, home-prepared foods have the dietary vitality that dogs evolved with, foods that retain their natural capacity to provide overall health and vigor. I have no scientific data to support this, but my guess is that an unprocessed diet that approximates the high protein diet of the wild canine will ultimately prove to be the best one for preventing renal disease. (Editor’s note: WDJ will publish an article on diets for kidney-compromised dogs in a few months.) Herbal therapies The list of herbs that may be helpful for aiding urinary problems is extensive. For starters, many herbs are diuretic, with a range of activity varying from slight to profound. Most conditions of the urinary tract benefit from an increased flow of urine, so almost any herb will be helpful in this regard. Further herbal selection depends on the specific condition – for example, one herb that has been used to treat kidney stones is bearberry or uva-ursi (Arcto-staphylos uva-ursi). My favorite herbal combination for non-specific urinary tract conditions, especially the recurring types that may be related to low grade infections, are dandelion root and Oregon grape root. Go, team! As I consider the various and sundry functions of the urinary system and how to best keep all its aspects healthy and functioning and in accord with other body systems, I can’t help but think that this is a prime example where a team approach may be the most beneficial. To be most effective, we need the diagnostic acumen of Western medicine, the services of a good, holistic dietitian (to help us provide the best balance by using whole foods), and an herbalist who is well informed on potential kidney toxicities as well as the benefits of the herbs. Finally, to provide the most beneficial treatment for a specific kidney disease, there will be occasions when Western medicine is simply more prudent and better than any of the alternatives available. Also With This Article Click here to view “Can Meat Cause Kidney Failure?” Click here to view “A Low-Protein ‘Kidney Diet’ is Not Always The Answer” Click here to view “Chronic Kidney Disease in Dogs” -Dr. Randy Kidd earned his DVM degree from Ohio State University and his PhD in Pathology/Clinical Pathology from Kansas State University. A past president of the American Holistic Veterinary Medical Association, he’s author of Dr. Kidd’s Guide to Herbal Dog Care and Dr. Kidd’s Guide to Herbal Cat Care.






the volume of the journal kidd 2005 anatomy of canine kidney