Caleb had been doing really well for a Bouvier about to turn 10, when his health took a mysterious dive last summer. We would learn that he was infected with an intestinal parasite called Giardia. But until he was correctly diagnosed and effectively treated, he suffered and his condition deteriorated.
A problematic Giardia infection is often overlooked or mistaken for other illnesses. Until only two or three years ago it was believed to be uncommon in dogs, says Dr. Andrew Peregrine, Associate Professor of Clinical Parasitology at the Ontario Veterinary College, University of Guelph.

However, recent studies have found that between 6 percent and 7 percent of dogs are infected with Giardia at any given time. And 8 out of 10 of these show no clinical signs of disease! Young dogs (up to one year old) may contract Giardia as much as six times more often than adults.
These findings suggest Giardia is a more significant issue for dogs than previously realized. It appears that dog people and practitioners have some catching up to do!
Elusive Giardia Symptoms
Caleb’s tale illustrates how humans can go astray when viewing Giardia through an outdated lens.
In early summer, Caleb had diarrhea for a day or two, but then it cleared up. He vomited once, and again a few weeks later. The diarrhea came and went again, but even his better-formed stools smelled bad. Our local clinic did a “float” test of a stool sample, telling my friend Janice and I that this could detect both worms and Giardia. When they found neither, we figured parasites weren’t Caleb’s problem.
The elusive pattern continued for weeks, then months. At times, Caleb went off his food. He’d wake up at night panting and clearly distressed, and sometimes couldn’t fall back to sleep for hours. His gut gurgled loudly and he released stinky gas – unusual, for him. I suspected intestinal cramps.
Then, almost overnight, his normally sweet breath became so foul that we had to open a car window for relief when he rode with us. It sometimes smelled like feces. Our vets insisted that Caleb probably had an oral problem, but like other dogs on a raw food diet, Caleb has healthy teeth and gums. Oddly, his chronically itchy skin and achy joints also seemed much worse, which logic said was unrelated to digestive issues; yet all this happened in tandem.
Caleb’s chiropractic vet noticed he had muscle-wasting. His weight had plummeted from 90 to 81 pounds; he was thin-skinned and ribby, although he ate well enough. She asked if he’d been checked for Giardia; we reported his negative results. Alarmed now that he might have cancer, she wanted to biopsy an irritated wart on his knee.
I just didn’t feel he had cancer. Afraid that surgery would add to his stress, we decided to hold off on it while continuing to search for other explanations.
Caleb’s homeopathic vet matched a remedy to his issues, and put him on probiotics and enzymes to help his digestion. When he did not improve, she tried to warn us that we should expect a 10-year-old dog to start having problems. “This isn’t aging,” I insisted. “Caleb is sick.”
Finally, Toronto holistic veterinarian Paul McCutcheon astutely asked what kind of Giardia test we’d had done. “Oh, no,” he said, by long-distance phone. “I don’t test in-clinic for Giardia anymore; it’s not reliable. Have an antigen test done right away. You’ll have to have it sent to a lab, but it’s the only way you’re really going to know whether he has it or not.”
So we did – and it came back positive. Giardia did not explain why Caleb’s itchy skin and achy joints seemed so much worse; we’d try to figure that out later. But thankfully, the parasite is treatable, and he’s now back to his old self.
About Dog Breath
Although vets don’t consider it a feature of the disease, the rise and fall of Caleb’s outrageously bad breath coincided with the course of his infection. Also, while his chronically itchy skin and arthritis appeared much worse when his digestive system went off the rails, they, too, eased off afterward. I offer the following suggestions.
First, it’s no wonder vets don’t look to breath quality as an indicator of health (except for possible oral problems). So many dogs have chronic halitosis that lots of people believe they naturally have bad breath! However, owners who’ve switched to raw or natural foods frequently report their dogs having pleasant, inoffensive breath like Caleb’s. We should not overlook our dogs’ breath as an important meter of wellness, particularly of the digestive system.
Second, like many dogs with autoimmune issues, Caleb has been on nutriceuticals such as glucosamine, MSM, marine oils, vitamins, and medicinal herbs for years. If he goes off them for long, his itchy skin and achy joints bother him more. Since Giardia interferes with the absorption of nutrients, it may also interfere with absorption of nutritional supplements. If so, this could further confuse the diagnostic picture when dogs in similar situations have Giardia infections.
What is Giardia?
Giardia is a microscopic, single-celled parasite that infects the guts of fish, birds, or mammals. It’s a major cause of diarrhea, and thereby a major cause of death of children under five in tropical and developing countries when there is poor hygiene and lack of water filtration. The Centers for Disease Control describes it as one of the most common causes of waterborne disease in the United States.
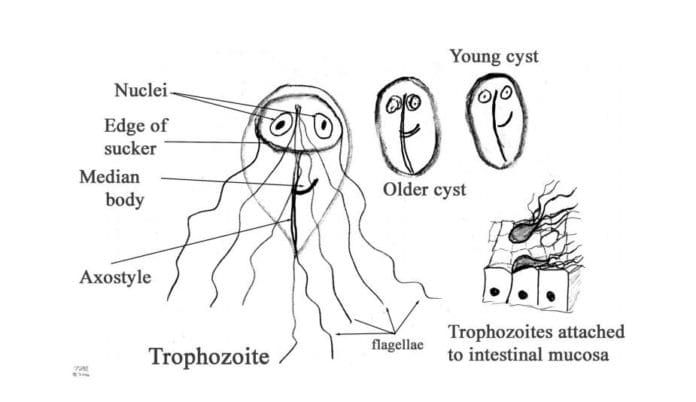
Giardia has two basic life-stages. As a “trophozoite,” it attaches itself to the lining of its host’s intestines with its sucker. There, it feeds, reproduces, and dies while actively colonizing its new dwelling-place.
Like any parasite, Giardia must seek new worlds to exploit. In its trophozoite form it can’t survive long outside a host’s digestive tract, so it transforms itself into individual “cysts” enclosed in resilient protective casings. In this form, the cysts exit an infected animal in the host’s excrement, chancing to end up somewhere they can remain viable until another host comes along.
The primary way to acquire Giardia is through oral contact with Giardia cysts. It happens mostly by drinking infected water, but, as you’ll see, it’s possible through other means, too. According to Dr. Peregrine, the ingestion of as few as 10 cysts can start an infection in dogs (and people). And the cycle continues.
To remain viable, Giardia cysts need a damp or wet environment in the right temperature range. They do best in woodland pools, ponds, streams, and lakes, but will also survive on a bedding of moist, organic matter such as a shaded forest floor. Dryness quickly destroys cysts, so they’re less a problem in deserts than elsewhere. They do well in humid warm climates. A rapid temperature drop to below freezing will kill most cysts as long as they’re actually caught in the ice, or in the part of the droppings or soil that becomes frozen.
But if they are protected, some cysts may survive for awhile even in extreme cold. For example, they might endure in fluid water beneath a layer of ice, or on soil insulated from frigid air by a good snow-cover. However, even in water cysts don’t live indefinitely; probably only for months, but not years, says Dr. Peregrine.
He adds, “Cysts that pass into water don’t multiply. They only multiply in the guts of animals.” In other words, in water, their numbers build up only through fecal matter that infected animals deposit in or near it.
This happens several ways. Infected land animals, including canids but not excluding infected humans, poop nearby and rains or melting snows wash the cysts into lakes or streams. Or water animals, such as beavers, excrete cyst-ridden feces right into the water. (Disease from Giardia is sometimes called “Beaver Fever,” but Dr. Peregrine thinks beavers may be unfairly blamed for the parasite’s success.) Giardia may also contaminate streams or lakes via untreated human sewage.
How Dogs Get Giardia
Dogs acquire Giardia primarily by drinking water that contains cysts. But chowing down infected feces will also do the trick!
However, not all types of Giardia affect dogs. Researchers now believe that it comes in different genotypes, and that most animals have at least one that’s limited to their own species. For example, one genotype is known to only infect dogs; another, only humans; yet a third is “shared” by both dogs and humans.
“Until recently,” says Dr. Peregrine, “we assumed that Giardia in dogs will always infect people, but it’s quite clear now that’s not the case. Some types of Giardia from dogs will infect people.” And sometimes, the opposite happens. He tells of a student who came home from Greece with a confirmed Giardia infection. A week later, the student’s dog became infected, too. “The dog almost certainly got Giardia as a result of drinking out of a toilet bowl,” he concludes. “So infection will go both ways! But not all human infections will infect dogs, and not all dog infections will infect people.”
How might we catch it from our dogs? If an infected dog’s anal area has traces of moisture, it could harbor cysts. As they dry up, the cysts lose viability. But in the meantime, if you brush against them and, yes, if they end up in your mouth, you may become infected. Being smooched by a dog dripping infected water from her muzzle might also expose you. However, there’s probably no point in getting too paranoid, as none of us can avoid Giardia completely.
The number of cysts a dog (or person) takes in affects his likelihood of getting infected; the more he ingests, the greater the odds are that it will happen. Environmental conditions influence this. For example, active streams or lakes can distribute cysts widely, whereas they may collect at the edges of quieter waters. Hot, dry spells can shrink smaller pools and ponds, concentrating existing cysts even closer together.
Giardia Might Look Like Something Else
Too often, vets and owners haven’t even thought to suspect Giardia as the cause of a dog’s diarrhea. Why not?
Dr. Peregrine suggests that vets have only just realized how common it is, thanks to the new data. “I think we didn’t understand it before. Seven percent of dogs (testing positive) is a very high figure!”
Furthermore, since the disease has no distinctive clinical signs of its own, it can mimic “just about anything that produces diarrhea!” Dr. Peregrine laughs. “Except diarrhea with blood. It’s extremely unusual to see blood with Giardia.”
And veterinarians tend to test first for what they believe is most common. Morag McMurray, DVM, of Kingston, Ontario, gives examples.
“If a dog comes in with skin and digestive problems, you’d look for a generalized inflammatory reaction first. Or, if he had hypothyroid and diarrhea, you’d thoroughly examine the thyroid first. If he had diarrhea but no vomiting, you’d wonder about a foreign body,” Dr. McMurray says.
These reasons may explain why vets have overlooked Giardia as a potential cause of disease. But it’s time for a change in perspective.
When should you suspect that Giardia may have infected your dog?
Signs of Giardia Infection
Over half of the approximately 80 percent of infected dogs without clinical signs may eventually clear it on their own. But the other 20 percent can become pretty unhappy campers. Giardia usually, but not always, affects dogs up to one year old, or unwell dogs with challenged immune systems, more harshly than it affects healthy dogs.
When a dog has signs, diarrhea may be the first and only one you’ll see. He may also throw up. But the diarrhea may be intermittent and vomiting occasional, making it hard to know whether your dog is ill or simply ate something untoward. Stool, whether loose or formed, may stink and contain mucous. If the parasite interferes with nutrient absorption, you may see weight loss, weakness, and muscle-wasting.
Abdominal pain can be another feature of the disease. Two humans I know who have had it insist, “It’s terrible! You have spasmodic intestinal cramps, like colic!” One reported a metallic taste in his mouth.
Giardia infections are not normally life-threatening. But the dangers of dehydration (from excessive diarrhea) or malabsorption are real. Ideally, we should look for the parasite well before things get to this point.
Different Giardia Tests
Giardia can be tough to identify in tests, and routine fecal examinations don’t normally detect the parasite. But several tests, with varying levels of accuracy, can. Repeat a test up to three times to be sure of negative results, or switch to one that’s more dependable. Many vets do in-clinic tests by default (they’re less expensive); if you want a specific test done by a lab, request it.
• The “ELISA” test. Considered the most reliable and becoming more popular. Looks for antigens. Goes to a lab. Most likely to get correct results the first time. Note that the ELISA test for Giardia will not detect other parasites or problems that your dog may have.
• The “float” test. Done in-clinic. Designed to look for worms. May also find cysts, but much more reliable when performed by technicians who are specifically trained to find Giardia this way.
• The “fecal smear.” Performed in-clinic on fresh feces; looks primarily for trophozoites before they die off. A less effective way to find cysts. Dr. McMurray calls it more of a rough guide/initial screening test.
• The “fluorescent antibody test” (FAb). Done at a lab. Generally more reliable than the fecal smear, but either can give false positives or negatives.
Testing for Giardia should not replace routine stool checks.
Giardia Treatment for Dogs
To treat, or not to treat? Just because your dog tests positive does not mean you should automatically treat him. If he has no clinical signs of disease, he may recover by himself. Using drugs if they’re not truly necessary may encourage Giardia to develop resistance, hampering our ability to help a severely infected dog down the line. (Possibly also for this reason, many doctors today do not treat Giardia-infected humans who have no symptoms.)
But sometimes it makes more sense to treat. Dogs like Caleb, overwhelmed by too many cysts, or whose weak immune systems can’t throw off the infection, need help. Also, if a dog lives with a human or another pet who has a compromised immune system (from cancer or AIDS, for example,) Giardia could hit that individual hard. To protect the immune-suppressed family member, Dr. Peregrine advises treating even Giardia-positive dogs who show no signs.
Owners may choose to treat their dogs for Giardia with conventional pharmaceutical drugs that kill the parasite in the gut, or by attempting to bring about intestinal balance through natural means. Whichever method you use, first carefully shampoo the hair around the dog’s rear end to remove any cysts that may be present.
The conventional pharmaceutical drugs used to kill Giardia are:
• Fenbendazole (Panacur, SafeGuard). Originally used for dogs as a de-wormer, it eliminates Giardia, too. Dr. Peregrine asserts that it’s generally more effective against Giardia than the old stand-by, metronidazole. It appears to have fewer side effects, too; consisting, if anything, of vomiting. “It’s probably one of the safest drugs we use in veterinary medicine,” he says. Individual dogs may be allergic to it.
The use of fenbendazole for Giardia is pretty new on the scene; two out of four practicing vets I consulted did not yet know of its use for that purpose. It’s given once a day for three days; if the dog still tests positive a month later, your vet will probably repeat treatment for a longer duration.
• Metronidazole (Flagyl). The drug of choice for years, it’s also the mainstay for treating Giardia in humans. It has a good success rate. However, it also has a rather daunting list of possible side effects: neurologic disorders, lethargy, weakness, effects on blood cells, damage to the liver, blood in urine, anorexia, vomiting, and diarrhea. It’s not considered safe for pregnant females. Still, many vets rely on it because it has worked well for them and they’ve had few, if any, problems with it.
Clinical experience suggests Giardia is becoming resistant to metronidazole, according to Dr. Peregrine. But he advocates keeping both drugs in use, because if everyone switched to fenbendazole, “sooner or later, we’re going to get resistance to that, too! We want to be sure, in 50 years’ time, we’ve still got one or two drugs that work.” For this reason, he advises against using either drug preventively for high-risk dogs.
• Natural methods. Grapefruit seed extract, oregano oil, and colloidal silver, among others, reputedly kill microbes, among them bacteria, viruses, and parasites. You can find these and other preparations in health food stores; follow instructions for treating parasites.
Although these methods may help with many things, it appears that holistically oriented folk haven’t yet reached consensus on their effectiveness against Giardia. In my survey of eight natural pet care books – some classic, others hot off the press – six didn’t mention Giardia at all; the seventh did, but only in passing. Only Mary Wulff-Tilford and Greg Tilford, in their book All You Ever Wanted to Know About Herbs for Pets, deal with it. After noting that herbal preparations for Giardia are “moderately successful at best,” they suggest combining low-alcohol tinctures of the following:
2 parts Oregon grape
2 parts licorice
2 parts cleavers
1 part garlic
They instruct giving this to the dog at least one hour before a meal. Dose at about ¼ teaspoon (1 milliliter) per 20 pounds of body weight, twice daily for up to 10 days; if the dog does not improve significantly by then, consult a holistic veterinarian.
Given the Tilfords’ cautions, perhaps we simply haven’t yet found the most effective nonconventional remedies for Giardia. If you do want to try one, remember it may take awhile to work – a consideration if your dog is already in poor condition or in pain.
Unfortunately, regardless of treatment, Giardia may persist. Dogs often reinfect themselves during therapy. Take precautions to reduce exposure. Also, your dog’s Giardia may be nonresponsive to the drug used. A change of drug might help. She may have an underlying issue suppressing her immune responses. Observe her closely and consult with your vet. Finally, neither dogs nor people develop immunity against Giardia. They, and we, can always have it again.
Giardia does not do permanent damage, but once it’s gone, a dog may need a little time to heal her intestinal lining. Probiotics can help with digestion in the meantime. Feed clean, non-irritating foods. If she had malabsorption, add nutritional supplements to help her regain what she lost.
Caleb did not respond to maximum doses of grapefruit seed extract and oregano oil, given for five days. But after two treatments with fenbendazole, he finally tested clear and regained his ideal weight. His digestion recovered over a few weeks, and his breath cleared along with it. Plus, his aggravated, itchy skin and achy joints calmed again to their “normal” level of irritation. Maybe the Giardia had interfered with his absorption of the supplements we give him to ease those problems.
A Word About Giardia Vaccines
Wyeth makes a vaccine called GiardiaVax,® which, the company claims, can prevent dogs from developing disease (diarrhea) caused by Giardia; it does not prevent infection. Dr. Peregrine conducted a study to look at whether the vaccine might also clear infections in dogs who have been nonresponsive to traditional treatment, but did not find that it had any effect on this. Further, he states that some people believe, on the basis of clinical experience, that the vaccine provides no significant benefit either preventively or therapeutically.
It should also be noted that the vaccine contains thimerosol, a preservative that contains mercury. Many holistic practitioners believe that preservatives that contain mercury can cause abnormalities of the nervous system, such as problems with coordination, vision, and learning
Giardia Prevention
You probably won’t be able to avoid Giardia completely, but you can certainly reduce your dog’s chances of contracting it.
• Support her immune system so that she can handle Giardia better. This requires a proper diet, regular exercise, enough natural light, and a minimum of problem stress. But even if she does contract the parasite, she still may not have an immune issue; a sufficiently high number of cysts could infect even the healthiest dog.
• Keep your dog’s living quarters and hindquarters clean and dry. Gentle shampoo followed by clean water will look after the dog personally; soaps lift cysts away from the body so you can rinse them off.
Concerning floors, here’s the most effective solution: flush them frequently with lots of plain water and let dry thoroughly before the dog comes back in. Concrete runs, especially, benefit from this. Many disinfectants don’t affect Giardia, and heavily soiled areas shield cysts from chemicals, anyway. Keeping clean is better. Steam-cleaning can also help as Giardia can’t survive temperatures over 60°C/152°F. Wash your hands well after clean-up.
• When you go out with your dog, avoid quiet waters where cysts may gather and to visit streams or bigger lakes, instead. Walk in woods after vernal pools have dried up in summer. Discourage him from eating feces. In your yard, see what you can do about standing water, but don’t worry about things like raised bird baths; if they’re too high for mammals to poop in, they likely won’t collect Giardia that could infect your dog.
What if, like us, you’re surrounded by swamp, or your dog loves the water and you don’t want to deny her that pleasure? Have your high-risk dog tested for Giardia annually. And if she develops diarrhea, think of Giardia first instead of last, and prompt your vet to look into it.
• Water treatment. Town water systems should deal with Giardia, but not all do. If yours doesn’t, you’re on a private well, or you take your dog camping, boil water for at least one minute to destroy cysts. Properly maintained ultraviolet light systems for private wells kill them. Filters with an absolute pore size of one micron, or that are rated “for cyst removal,” will snag them. Remember: you can’t detect Giardia just by looking or sniffing at water. Cysts may dwell there even if it appears pristine and delicious!
Finally, don’t get discouraged if you’re trying to do everything responsibly but your dog still gets Giardia. There’s no such thing as zero risk with the parasite; just do what you can, be realistic, and get out there and have fun with your dog.
GIARDIA IN DOGS: OVERVIEW
1. Consider Giardia first rather than last as a possible cause of your dog’s diarrhea.
2. Request that your veterinarian send a sample away for an antigen test, or, if they’re doing a “float,” ask for a technician who’s been specifically trained to find Giardia that way.
3. Don’t let your dog drink from the toilet! They can become infected by an infected person this way. Remember, an infected person (or dog) may not exhibit symptoms.
4. Ask your vet to make Giardia part of your dog’s annual parasite test.
Susan Weinstein is a freelance writer with a strong interest in animals and holistic healthcare. Presently, she is working on a book about pets and stress with Paul McCutcheon, DVM. Weinstein and Caleb live in Grafton, Ontario.